Volume reduction in amygdala tracks with depression relief after ketamine infusions
Researchers have identified a specific structural change in the brain that appears to track with the relief of depressive symptoms following ketamine treatment. In a group of patients with treatment-resistant depression, a reduction in the volume of a specific sub-region of the amygdala was linked to a decrease in feelings of unhappiness and unease. These findings were published in the Journal of Psychiatric Research.
Major depressive disorder is a pervasive condition that affects millions of individuals globally. Standard treatments, such as selective serotonin reuptake inhibitors, are effective for many. However, roughly thirty percent of patients do not experience adequate relief even after trying multiple different medications. This condition is categorized as treatment-resistant depression.
Ketamine has emerged in recent years as a potent alternative for these difficult-to-treat cases. It is an anesthetic drug that functions differently from traditional antidepressants. Clinical trials have repeatedly demonstrated that it can provide rapid relief for severe depression. Despite its proven efficacy, the precise biological mechanisms by which ketamine alters the brain to improve mood remain largely unknown.
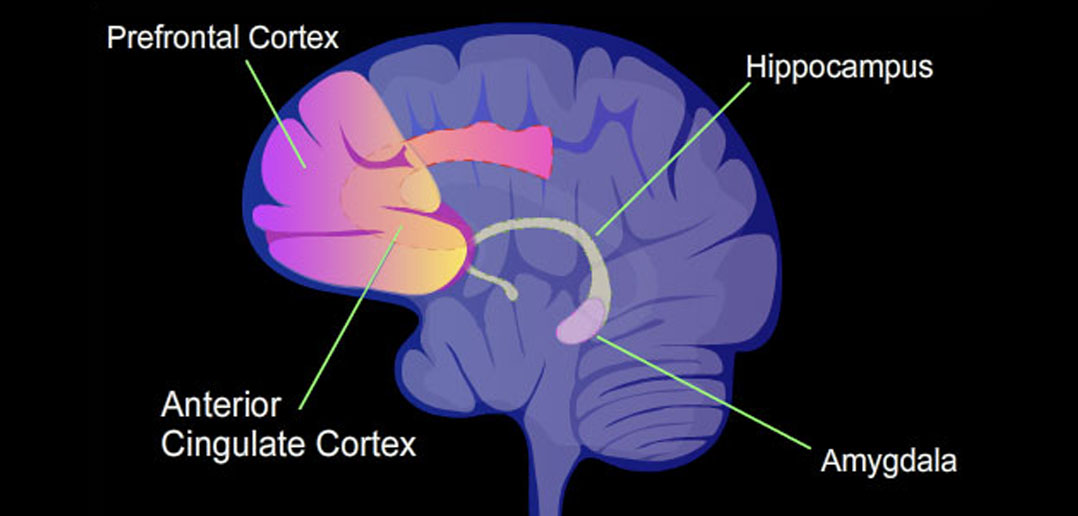
The amygdala is a small, almond-shaped structure located deep within the temporal lobes of the brain. It is widely recognized as a central hub for processing emotions, particularly fear and negative stimuli. In people suffering from depression, this brain region often exhibits excessive activity. Neuroscientists have long suspected that this hyperactivity contributes to the persistent negative emotional state associated with the disorder.
Previous research using functional magnetic resonance imaging has supported this idea. Studies have shown that ketamine administration can dampen this excessive activity in the amygdala. However, the relationship between the physical size, or volume, of the amygdala and the therapeutic effects of ketamine has been less clear.
Past attempts to measure amygdalar volume in depressed patients have yielded inconsistent results. Some studies reported shrinkage, while others reported enlargement. A potential reason for these discrepancies is that the amygdala is not a single, uniform object. It is a complex of multiple distinct nuclei, or subfields. These subfields have different cellular structures and connect to different parts of the brain.
The research team was led by Kengo Yonezawa and Shinichiro Nakajima from the Department of Neuropsychiatry at Keio University School of Medicine in Tokyo, Japan. They hypothesized that looking at the amygdala as a whole might obscure important changes occurring within its specific internal structures. They proposed that changes in the volume of specific subfields might correlate with how well a patient responds to ketamine.
To test this hypothesis, the investigators utilized data from a rigorous clinical trial. The study was a double-blind, randomized, placebo-controlled trial. This design is the gold standard in medical research because it minimizes bias. Participants were adults between the ages of 20 and 59 who had failed to respond to at least two different antidepressants.
The study enrolled 34 participants with treatment-resistant depression. These individuals were randomly assigned to receive either intravenous ketamine or a saline placebo. The infusions were administered twice a week for a period of two weeks.
The researchers used high-resolution magnetic resonance imaging to scan the brains of the participants. Scans were taken at two specific time points. The first scan occurred before the treatment began. The second scan took place approximately five to six days after the final infusion.
The team employed advanced software called FreeSurfer to analyze the brain images. This automated tool allowed them to digitally segment the amygdala into three distinct functional sub-regions. These were the laterobasal nuclei, the centromedial nuclei, and the superficial nuclei.
The laterobasal nuclei are considered the primary input centers of the amygdala. They receive sensory information from the cortex and other brain areas. The centromedial nuclei act as the output center, sending signals to the brainstem to trigger behavioral responses. The superficial nuclei are connected to the olfactory cortex.
Depressive symptoms were measured using the Montgomery Åsberg Depression Rating Scale. The researchers looked at the total score, but they also broke the scores down into subdomains. These subdomains included dysphoria, which covers sadness and pessimistic thoughts; retardation, which covers lethargy and lack of feeling; and vegetative symptoms, such as sleep and appetite changes.
The analysis revealed a specific statistical interaction. In the group of patients who received ketamine, there was a positive association between the change in volume of the right laterobasal nuclei and the change in dysphoria scores. Specifically, as the volume of this brain region decreased, the patients’ reported feelings of sadness and unease also decreased.
This correlation was exclusive to the ketamine group. Patients in the placebo group did not show this relationship between brain structure and symptom improvement. This distinction suggests that the observation is not merely a general feature of feeling better. It implies a specific neurobiological effect induced by the drug.
The researchers did not find similar associations in the other subfields of the amygdala. The left side of the amygdala also did not show this specific correlation. The connection was isolated to the right laterobasal nuclei and the improvement of dysphoric symptoms.
These findings align with the theory that the amygdala is overactive in depression. The laterobasal nuclei receive inputs from the prefrontal cortex. This is the part of the brain responsible for higher-order thinking and regulation. In depression, the communication between the prefrontal cortex and the amygdala is often impaired.
The authors suggest that ketamine may help restore normal function to the prefrontal cortex. This restoration allows for better “top-down” control of the amygdala. The observed reduction in volume might represent a physical manifestation of this reduced hyperactivity. Essentially, as the region becomes less overactive, it may undergo subtle structural changes that reflect a more normalized state.
It is worth noting that the study did not find a significant difference in the average volume change between the ketamine group and the placebo group when looking at the participants as a whole. The effect was only visible when looking at the correlation with symptom improvement. This means ketamine did not simply shrink the amygdala in everyone. Rather, the shrinkage tracked with who got better.
There are several limitations to this study that require consideration. The sample size was relatively small. Due to logistical issues and dropouts, the final analysis included eleven patients in the ketamine group and fifteen in the placebo group. Small sample sizes can sometimes lead to results that are not reproducible in larger populations.
Another limitation is that the participants remained on their standard antidepressant medications during the trial. While this reflects real-world clinical practice, it introduces a variable. It is theoretically possible that the background medications influenced the brain structure in some way.
The study was also exploratory in nature. The researchers examined multiple brain regions and symptom scores. While they used statistical methods to validate their findings, larger studies are needed to confirm these results.
Additionally, the study did not include a healthy control group. Without healthy subjects for comparison, it is difficult to know if the amygdalar volumes in these patients were abnormal to begin with. It is also unclear whether the volume reduction represents a return to a “normal” size or a change to a new state.
The duration of the study was short. The second MRI scan was taken less than a week after the final treatment. It remains unknown whether these structural changes persist over time. It is also unclear if the volume of the amygdala would return to its previous state if the depressive symptoms recurred.
Despite these caveats, the research offers a new perspective on how ketamine treats depression. It moves beyond general ideas of “chemical imbalance” to look at specific structural changes in emotional processing centers. The identification of the right laterobasal nuclei as a region of interest provides a target for future investigations.
Understanding these biological markers is essential for the development of personalized medicine in psychiatry. If doctors can identify which brain structures need to change for recovery to occur, they may be able to predict which patients will respond to ketamine. This could spare patients from undergoing treatments that are unlikely to work for their specific biology.
The study, “The association between amygdalar volume changes and depressive symptom improvements after repeated ketamine infusion in treatment-resistant depression: a double-blind, randomized, placebo-controlled trial with the following open-label study,” was authored by Kengo Yonezawa, Shinichiro Nakajima, Nobuaki Hondo, Yohei Ohtani, Kie Nomoto-Takahashi, Taisuke Yatomi, Sota Tomiyama, Nobuhiro Nagai, Keisuke Kusudo, Koki Takahashi, Shiori Honda, Sotaro Moriyama, Takashige Yamada, Shinsuke Koike, Hiroyuki Uchida, and Hideaki Tani.
 Each has pros and cons.
Each has pros and cons. 

 It's looking like rush hour up there.
It's looking like rush hour up there.








 Welcome cousin!
Welcome cousin!


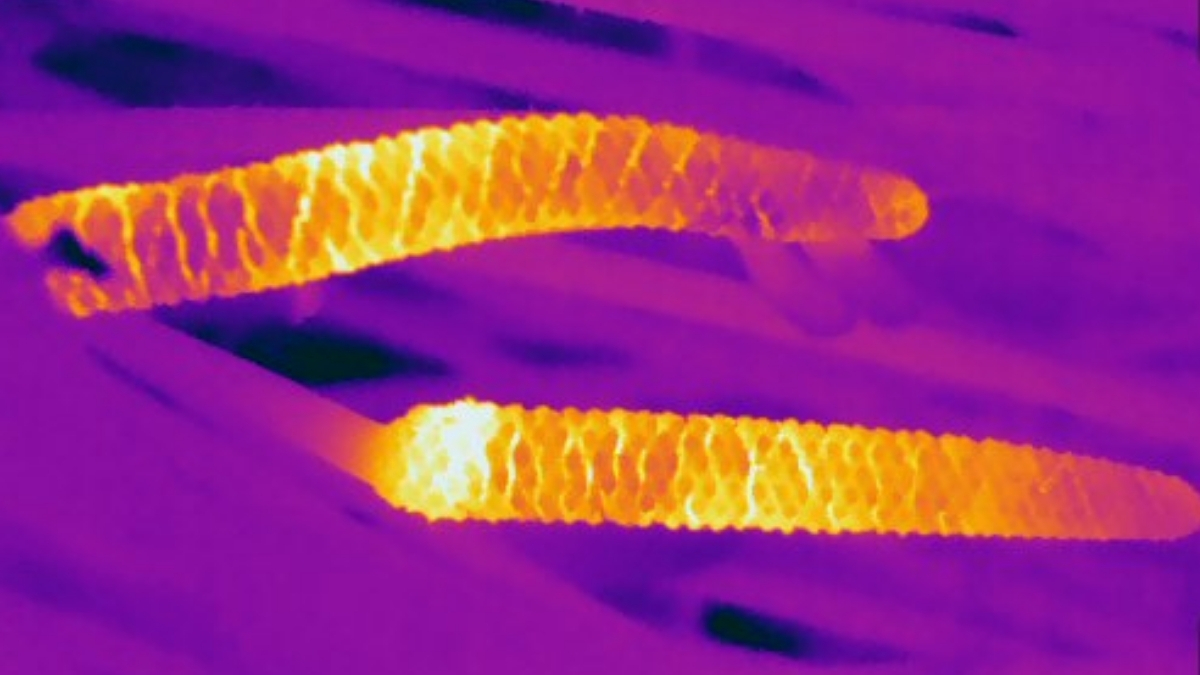
 Power up.
Power up.



 Here it comes!
Here it comes!
 Is there a better approach?
Is there a better approach? Decades of assumptions could be wrong.
Decades of assumptions could be wrong. That's not even a worst-case scenario.
That's not even a worst-case scenario.
 It's not just a hallucinogen.
It's not just a hallucinogen.




 *Stares intently*
*Stares intently*










 Lake Manly returns.
Lake Manly returns. A significant clue.
A significant clue.




 Long before there were flowers.
Long before there were flowers. Germans have a word for this kind of thing.
Germans have a word for this kind of thing. Tylos is one weird world.
Tylos is one weird world.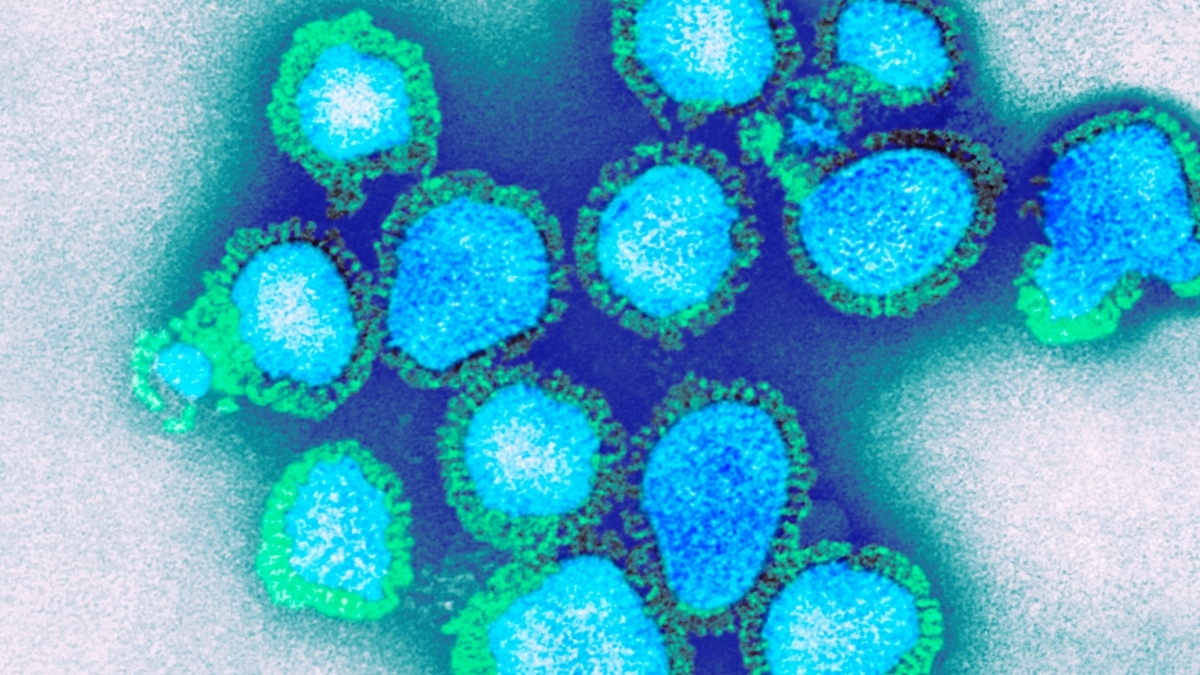 It's not unprecedented.
It's not unprecedented.  It’s important to get help.
It’s important to get help.
 Take note, ChatGPT.
Take note, ChatGPT.

 Why was she buried this way?
Why was she buried this way?
 We have to rethink this.
We have to rethink this.


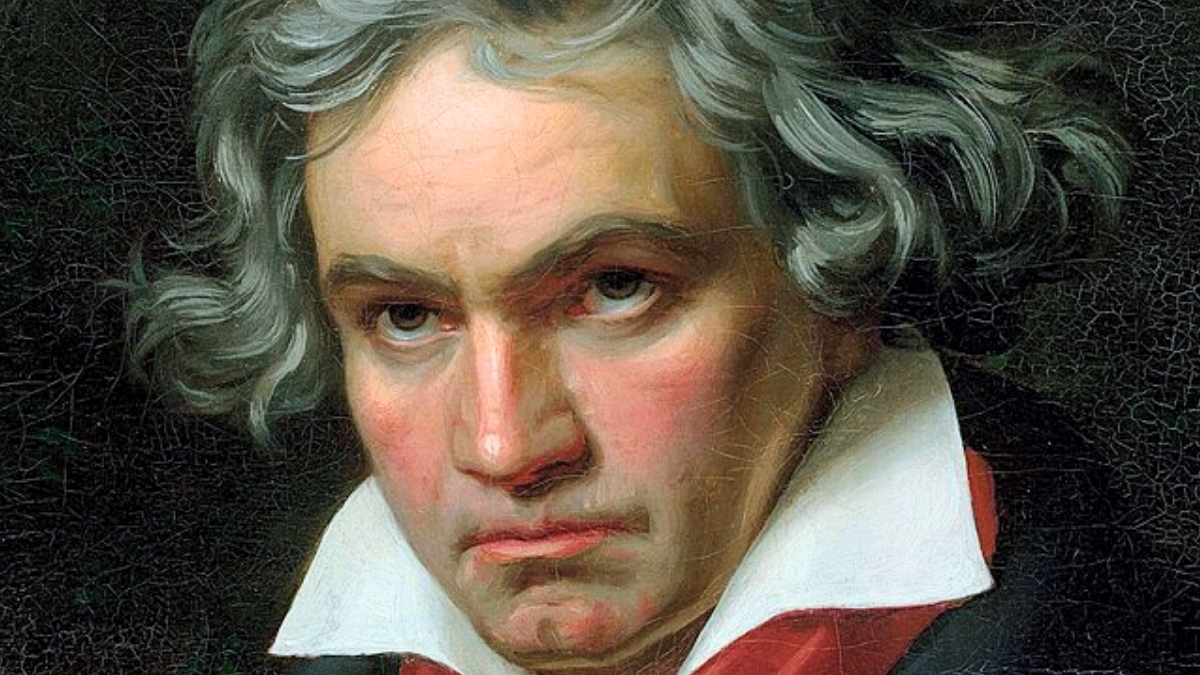 A tragic irony.
A tragic irony.
 And you can view it now.
And you can view it now.