Extra virgin olive oil supplementation reduces neuroinflammation in obese rats
A study of obese rats in Brazil found that adding extra virgin olive oil to their diets reduced inflammation in the arcuate nucleus of the hypothalamus, prevented them from gaining excessive weight, and improved a number of metabolic parameters. The research was published in Nutritional Neuroscience.
Extra virgin olive oil is the highest-quality form of olive oil, obtained directly from olives using only mechanical methods without any chemical refining. It must meet strict standards for acidity (less than 0.8%) and pass sensory tests for taste and aroma. Extra virgin olive oil retains the natural flavors and antioxidants of the olive fruit because it is cold-pressed and minimally processed.
Regular olive oil, in contrast, is usually a blend of refined olive oils and some virgin oil to improve flavor. Refining removes impurities but also strips away many beneficial compounds, making it milder in taste and lower in nutrients.
Extra virgin olive oil has a distinct fruity, peppery, or slightly bitter taste depending on the olive variety and ripeness. It is rich in heart-healthy monounsaturated fats, and its minimal processing preserves high levels of polyphenols and vitamin E, which have antioxidant and anti-inflammatory properties. Regular olive oil is lighter in flavor, more stable at high temperatures, and often used for frying or cooking in bulk. Extra virgin olive oil, however, is a better choice for salads, drizzling, and dishes where its aroma can be appreciated.
Study author Ariadni Peres and her colleagues wanted to explore whether extra virgin olive oil can be used to treat obesity. More specifically, they wanted to explore the effects of EVOO supplementation on various metabolic parameters, satiety, and hypothalamic inflammation—all hallmarks of diet-induced obesity.
These authors conducted a study on 21-day-old Wistar rats. Wistar rats are a common albino laboratory rat strain widely used in biomedical research because of their calm temperament and well-documented physiology. They were kept in cages with up to 4 same-sex animals per cage.
The rats were divided into 4 groups. The first group received regular rat food (standard chow). The second group received the same type of regular food, but also EVOO supplementation. The third group was on a high-fat diet (HFD), eating food with an increased content of fats. Finally, the fourth group received the high-fat diet and extra virgin olive oil supplementation. Olive oil supplementation was administered daily by gavage.
The standard chow was composed of 11.9% fat, 58.8% carbohydrate, and 29.2% protein, with an energy density of 3.86 Kcal/g. In contrast, the high-fat diet contained 64% of its calories from fat. Extra virgin olive oil supplementation was 1.3 mL/Kg body weight.
The rats were kept on this diet throughout the study. On day 61 of their lives, study authors took the rats’ blood samples to determine their fasting glucose levels. On days 63-65 the rats completed a number of behavioral satiety tests. On day 70, the rats were euthanized, allowing researchers to analyze their tissues and conduct various biochemical analyses.
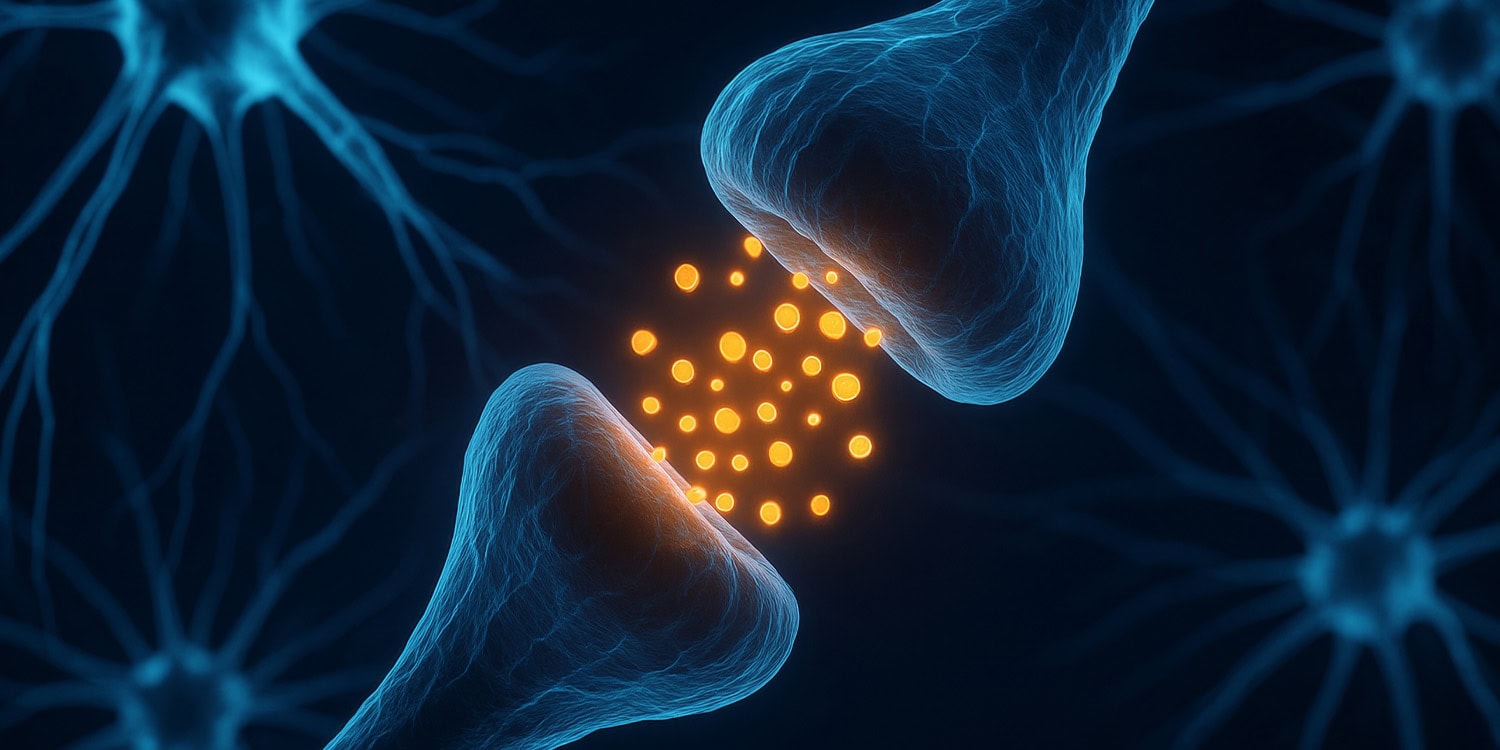
Results showed that, as expected, rats fed the high-fat diet became obese. However, extra virgin olive oil supplementation prevented the excessive weight-gain caused by the high-fat diet. It also reduced the level of inflammation in the arcuate nucleus of the hypothalamus and improved a number of other metabolic parameters in rats fed a high-fat diet.
“Our results demonstrate that extra virgin olive oil supplementation seemed promising, improving hypothalamic inflammation in obese animals, [and] therefore might lead to the restoration of adverse metabolic consequences,” the study authors concluded.
The study sheds light on the effects of extra virgin olive oil supplementation on rats fed a high-fat diet. However, it should be noted that this study was conducted on rats, not on humans. While rats and humans share many physiological similarities, they are still very different species. Effects on humans might differ.
The paper, “Extra virgin olive oil supplementation reduces inflammation in the arcuate nucleus of the hypothalamus and improves metabolic parameters in obese rats,” was authored by Ariadni Peres, Ricardo Dantas, Aline Ferreira, Ana Caroline Silveira, Giovana Raphaelli, Laís Felipe, Letícia Souza, Mariana Costa, Alessandra Machado, Diorlon Machado, Rodrigo Herrmann, Jade de Oliveira, Carlos Alexandre Netto, Angela Wyse, Carla Dalmaz, and Rachel Bast.