Depression and anxiety linked to stronger inflammation in sexual minority adults compared to heterosexuals
A new study published in the journal Brain, Behavior, and Immunity provides evidence that sexual minority adults may experience a distinct physiological reaction to mental health challenges compared to heterosexual adults. The findings indicate that while depression and anxiety are more common in sexual minority populations, these conditions are also accompanied by stronger inflammatory responses for this group.
Health disparities affecting lesbian, gay, bisexual, and other non-heterosexual individuals are well-documented in medical literature. Statistics indicate that these groups face a higher risk for chronic physical conditions like heart disease, asthma, and diabetes compared to heterosexual adults. They also report rates of anxiety and depression that are often significantly higher than those seen in the general population.
Scientists often utilize the minority stress theory to explain these gaps. This framework suggests that the unique social stressors faced by marginalized groups create a burden that wears down physical health over time.
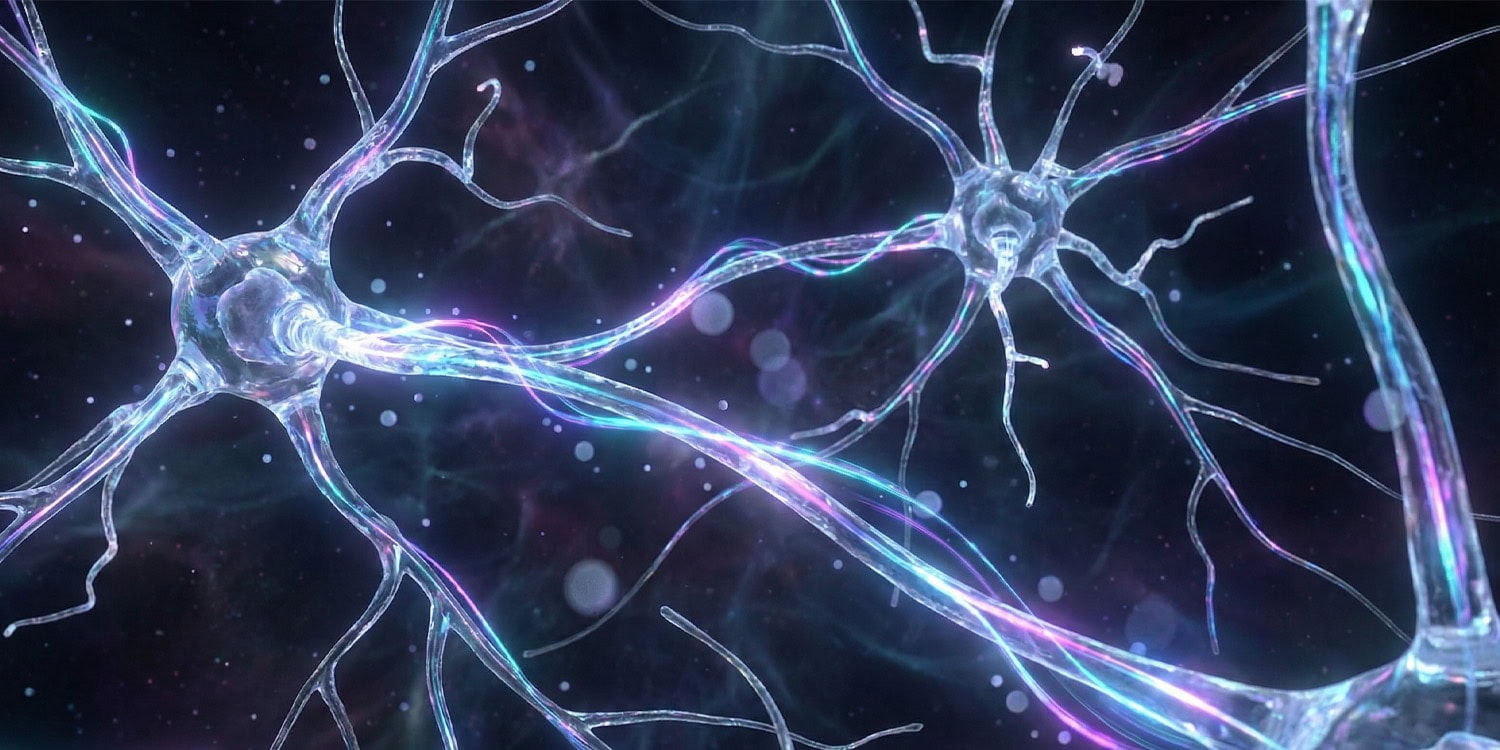
A key biological mechanism that might explain how stress becomes physical illness is inflammation. While acute inflammation is a necessary immune response to heal injuries or fight infection, chronic low-grade inflammation is damaging to the body.
Elevated levels of inflammatory markers are linked to a range of age-related conditions, including cardiovascular disease and cognitive decline. This process is sometimes referred to as “inflammaging,” where chronic inflammation contributes to accelerated biological aging.
“Sexual minority adults face well-documented disparities in both mental and physical health, including higher rates of depression, anxiety, and chronic conditions like cardiovascular disease,” said study author Lisa M. Christian, a professor and member of the Institute of Brain, Behavior and Immunology at The Ohio State University.
“While minority stress theory provides a framework for understanding these disparities, there has been very little research on the biological mechanisms that link psychological distress to physical health in this population. Specifically, data on inflammation, a key pathway to chronic disease, are scarce. Our study aimed to address this gap by examining whether depressive symptoms and anxiety are associated with greater inflammatory responses among sexual minority adults compared to heterosexual adults.”
The research team analyzed data from the National Couples’ Health and Time Study (NCHAT). This project involves a population-representative sample of married and cohabiting adults across the United States.
“This study utilizes data from Wave 1 of the National Couples’ Heath and Time (NCHAT) Stress Biology Study (NCHAT-BIO),” Christian noted. “NCHAT-BIO the first US-based study focused on stress biology within a large, diverse sample of married/cohabiting sexual minority and heterosexual adults.”
“NCHAT-BIO capitalized on the unique opportunity of NCHAT, a population-representative US sample which intentionally oversampled sexual minority respondents. Wave 1 NCHAT-BIO data have been deposited at ICPSR for public release to all researchers. We encourage interested researchers to take advantage of this unique and impactful dataset.”
The researchers focused on a subset of participants who provided biological samples. The final analysis included 572 participants. There were 321 individuals who identified as heterosexual and 251 who identified as sexual minorities, a group that included lesbian, gay, bisexual, and other non-heterosexual identities.
Participants completed detailed surveys assessing their mental health. To measure anxiety, they used the Generalized Anxiety Disorder scale (GAD-7). This tool asks respondents how often they have been bothered by problems such as feeling nervous or being unable to stop worrying.
To evaluate depressive symptoms, the researchers used the Center for Epidemiologic Studies Depression scale (CES-D 10). This measure asks participants how often they felt specific ways, such as fearful or lonely, during the past week.
The study also assessed adverse childhood experiences (ACEs) to understand early life stress. Participants reported if they had experienced events before age 18 such as abuse, neglect, household dysfunction, or parental incarceration.
Additionally, the survey asked about experiences of everyday discrimination and aggression. This included questions about being treated with less respect, being harassed, or facing physical attacks.
To measure biological markers, participants provided dried blood spots. They collected these samples at home by pricking a finger and placing blood drops on a special collection card. The researchers analyzed these samples for two specific markers of systemic inflammation: Interleukin-6 (IL-6) and C-reactive protein (CRP).
IL-6 is a cytokine that signals the immune system to respond to trauma or infection, while CRP is a protein produced by the liver in response to inflammation. Higher levels of these markers generally indicate a state of higher systemic inflammation.
The results showed that sexual minority participants reported higher levels of both anxiety and depressive symptoms compared to heterosexual participants. This aligns with prior statistics regarding mental health in these communities.
A statistical analysis revealed that this difference was partially explained by a higher number of adverse childhood experiences among the sexual minority group. Sexual minority respondents reported an average ACE score that was significantly higher than that of heterosexual respondents.
The most distinct finding emerged when the researchers analyzed the relationship between these mental health symptoms and inflammation levels. The data revealed a physiological pattern for sexual minority adults that was absent in heterosexual adults.
Among sexual minority participants, higher scores on the depression scale were associated with higher levels of both IL-6 and CRP. Similarly, higher anxiety scores were linked to higher CRP levels in the sexual minority group.
“We expected sexual minority adults to have higher depression and anxiety, which is consistent with prior research,” Christian told PsyPost. “What surprised us was the pattern of inflammatory response: sexual minority adults showed greater elevations in CRP with rising anxiety and depression. This effect was not seen in heterosexual adults. This suggests a unique physiological sensitivity among sexual minority individuals that warrants further investigation.”
The researchers adjusted their statistical models to account for potential confounding factors. They controlled for age, race, sex assigned at birth, education level, and existing health conditions.
They also ran sensitivity analyses that included body mass index and tobacco use. Even with these behavioral and physical factors included, the connection between distress and inflammation remained significant for sexual minority adults.
The study authors propose that this heightened inflammatory response is not an inherent trait of sexual minority individuals. Instead, it is likely a consequence of living in a marginalized social context.
Chronic exposure to stressors, such as discrimination or the threat of judgment, can sensitize the immune system. This sensitization means that when an individual experiences depression or anxiety, their body mounts a stronger inflammatory defense than it otherwise would.
This sensitization contributes to a “double burden” for sexual minority adults. First, they experience a higher prevalence of anxiety and depression, largely due to adverse childhood experiences and minority stress.
Second, when they do experience these symptoms, their bodies react with greater inflammation. Over time, even modest elevations in markers like CRP and IL-6 can increase the risk for chronic illnesses, potentially explaining some of the physical health disparities seen in this population.
“The main takeaway is that sexual minority adults not only experience higher rates of depression and anxiety but also show stronger inflammatory responses when they do,” Christian explained. “Even modest elevations in inflammation can increase long-term risk for chronic illnesses. This means that mental health challenges in sexual minority populations may have ripple effects on physical health, underscoring the importance of integrated care and targeted prevention efforts.”
There are some limitations to consider. The study used data collected at a single point in time for the survey, with blood samples collected several months later. This timeline makes it difficult to determine causality.
It is possible that inflammation exacerbates mood symptoms, rather than the other way around. The gap between the survey and the blood collection introduces some statistical noise, though the findings remained robust despite this.
“It is notable that the current effects in sexual minority adults were observed despite the presence of this statistical ‘noise,'” Christian said. “However, future studies in which time of collection is both simultaneous and longitudinal would be ideal.”
“Indeed, it is plausible that the presence of associations between inflammation and mental health indicators among sexual minority respondents, but not heterosexual respondents, is a function of greater chronicity of symptoms among sexual minority respondents. This could not be tested in the current analyses.”
The sample consisted entirely of married or cohabiting adults. People who are partnered often have better health outcomes and more social support than single individuals. This means the results might not fully reflect the experiences of unpartnered sexual minority adults.
The researchers also caution against interpreting these results to mean that sexual minority adults are inherently less healthy. “There is nothing problematic or unhealthy about being a sexual minority,” Christian told PsyPost.
“The differences we observed reflect the physiological costs of living in a society where sexual minority individuals are exposed to higher levels of stress, discrimination, and adversity, not something intrinsic to their identity. In other words, the burden comes from external exposures, not from who people are.”
The researchers have received funding from the National Institute on Aging to extend this work into a longitudinal study. They intend to examine how inflammatory markers change as the participants age. They also plan to look at epigenetic aging, which uses DNA methylation to measure biological age. This will help determine if the observed inflammation is translating into accelerated aging at the cellular level.
“This manuscript is part of a larger longitudinal study,” Christian said. “As with NCHAT-BIO Wave 1 data, assay results from Wave 3 will be made publicly available to other researchers through ICPSR alongside the survey, time diary, and contextual data from NCHAT Waves 1 through 3, and biological data from NCHAT-BIO Wave 1. Together, these resources will provide an exceptional dataset for future researchers.”
The study, “Sexual minority adults exhibit greater inflammation than heterosexual adults in the context of depressive symptoms and Anxiety: Pathways to health disparities,” was authored by Lisa M. Christian, Rebecca R. Andridge, Juan Peng, Nithya P. Kasibhatla, Thomas W. McDade, Tessa Blevins, Steve W. Cole, Wendy D. Manning, and Claire M. Kamp Dush.