Google’s AI co-scientist just solved a biological mystery that took humans a decade
Can artificial intelligence function as a partner in scientific discovery, capable of generating novel, testable hypotheses that rival those of human experts? Two recent studies highlight how a specialized AI developed by Google not only identified drug candidates that showed significant anti-fibrotic activity in a laboratory model of chronic liver disease but also independently deduced a complex mechanism of bacterial gene transfer that had taken human scientists years to solve.
The process of scientific discovery has traditionally relied on human ingenuity, combining deep expertise with creative insight to formulate new questions and design experiments. However, the sheer volume of published research makes it challenging for any single scientist to connect disparate ideas across different fields. A new wave of artificial intelligence tools aims to address this challenge by augmenting, and accelerating, human-led research.
One such tool is Google’s AI co-scientist, which its developers hope will significantly alter the landscape of biomedical research. Recent studies published in Advanced Science and Cell provide early evidence of this potential, showing the system’s ability to not only sift through vast datasets but also to engage in a reasoning process that can lead to high-impact discoveries.
Google’s AI Co-scientist: A Multi-Agent System for Discovery
Google’s AI co-scientist is a multi-agent system built upon the Gemini 2.0 large language model, designed to mirror the iterative process of the scientific method. It operates not as a single entity, but as a team of specialized AI agents working together. This structure is intended to help scientists generate new research ideas, create detailed proposals, and plan experiments.
The system operates through a “scientist-in-the-loop” model, where human experts can provide initial research goals, offer feedback, and guide the AI’s exploration using natural language. The specialized agents each handle a distinct part of the scientific reasoning process. The Generation Agent acts as a brainstormer, exploring scientific literature and engaging in simulated debates to produce initial ideas. The Reflection Agent serves as a peer reviewer, critically assessing these ideas for quality, novelty, and plausibility.
Other agents contribute to refining the output. The Ranking Agent runs an Elo-based tournament, similar to chess rankings, to prioritize the most promising hypotheses. The Evolution Agent works to improve top-ranked ideas by combining concepts or thinking in unconventional ways. A Meta-review Agent synthesizes all the feedback to improve the performance of the other agents over time. This collaborative, self-improving cycle is designed to produce increasingly novel and high-quality scientific insights.
AI Pinpoints New Drug Candidates for Liver Fibrosis
In the study published in Advanced Science, researchers partnered with Google to explore new ways of treating liver fibrosis, a progressive condition marked by excessive scarring in the liver. Current treatment options are extremely limited, in part because existing models for studying the disease do not accurately replicate how fibrosis develops in the human liver. These limitations have hindered drug development for years.
To address this gap, the research team asked the AI co-scientist to generate new, testable hypotheses for treating liver fibrosis. Specifically, they tasked the AI with exploring how epigenomic mechanisms—chemical changes that influence gene activity without altering the DNA sequence—might be targeted to reduce or reverse fibrosis.
“For the data used in the paper, we provided a single prompt and received a response from AI co-scientist, which are shown in supplemental data file 1,” explained Gary Peltz, a professor at Stanford University School of Medicine. “The prompt was carefully prepared, providing the area (epigenomic effects in liver fibrosis) and experimental methods (use of our hepatic organoids) to focus on. However, in most cases, it is important to iteratively engage with an AI in order to better define the question and enable it to provide a more complete answer.”
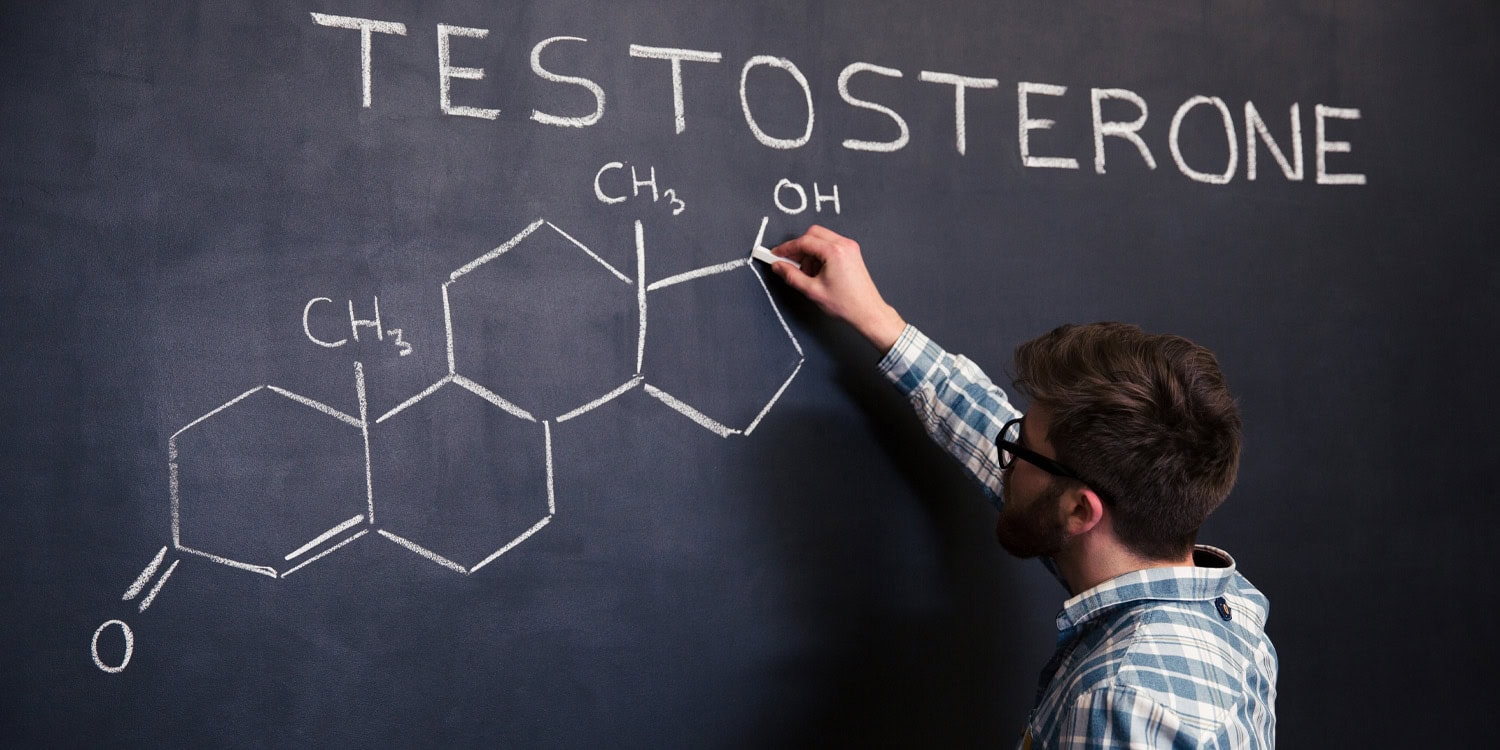
The AI system scanned the scientific literature and proposed that three classes of epigenomic regulators could be promising targets for anti-fibrotic therapy: histone deacetylases (HDACs), DNA methyltransferase 1 (DNMT1), and bromodomain protein 4 (BRD4). It also outlined experimental techniques for testing these ideas, such as single-cell RNA sequencing to track how the drugs might affect different cell populations. The researchers incorporated these suggestions into their experimental design.
To test the AI’s proposals, the team used a laboratory system based on human hepatic organoids—three-dimensional cell cultures derived from stem cells that resemble key features of the human liver. These mini-organs contain a mix of liver cell types and can model fibrosis when exposed to fibrotic triggers like TGF-beta, a molecule known to promote scarring. The organoid system allowed researchers to assess not just whether a drug could reduce fibrosis, but also whether it would be toxic or promote regeneration of liver tissue.
The findings provided evidence that two of the drug classes proposed by AI (HDAC inhibitors and BRD4 inhibitors) showed strong anti-fibrotic effects. One of the tested compounds, Vorinostat, is an FDA-approved cancer drug. In the organoid model, it not only suppressed fibrosis but also appeared to stimulate the growth of healthy liver cells.
“Since I was working on the text for a grant submission in this area, I was surprised by the AI co-scientist output,” Peltz told PsyPost.
In particular, Peltz was struck by how little prior research had explored this potential. After checking PubMed, he found over 180,000 papers on liver fibrosis in general, but only seven that mentioned Vorinostat in this context. Of those, four turned out to be unrelated to fibrosis, and another only referenced the drug in a data table without actually testing it. That left just two studies directly investigating Vorinostat for liver fibrosis.
While the HDAC and BRD4 inhibitors showed promising effects, the third AI-recommended class, DNMT1 inhibitors, did not. One compound in this category was too toxic to the organoids to be considered viable for further study.
To evaluate the AI’s performance, Peltz also selected two additional drug targets for comparison based on existing literature. These were chosen precisely because they had more published support suggesting they might work against fibrosis.
But when tested in the same organoid system, the inhibitors targeting those well-supported pathways did not reduce fibrosis. This outcome suggested that the AI was able to surface potentially effective treatments that human researchers might have missed, despite extensive literature reviews.
Looking ahead, Peltz said his team is “developing additional data with our liver organoid system to determine if Vorinostat can be effective for reducing an established fibrosis, and we are talking with some organizations and drug companies about the potential for Vorinostat being tested as an anti-fibrotic agent.”
An AI Recapitulates a Decade-Long Discovery in Days
In a separate demonstration of its reasoning power, the AI co-scientist was challenged to solve a biological mystery that had taken a team at Imperial College London over a decade to unravel. The research, published in Cell, focused on a peculiar family of mobile genetic elements in bacteria known as capsid-forming phage-inducible chromosomal islands, or cf-PICIs.
Scientists were puzzled by how identical cf-PICIs were found in many different species of bacteria. This was unexpected because these elements rely on viruses called phages to spread, and phages typically have a very narrow host range, often infecting only a single species or strain. The human research team had already solved the puzzle through years of complex experiments, but their findings were not yet public.
They had discovered a novel mechanism they termed “tail piracy,” where cf-PICIs produce their own DNA-filled “heads” (capsids) but lack tails. These tailless particles are then released and can hijack tails from a wide variety of other phages infecting different bacterial species, creating chimeric infectious particles that can inject the cf-PICI’s genetic material into a new host.
To test the AI co-scientist, the researchers provided it only with publicly available information from before their discovery was made and posed the same question: how do identical cf-PICIs spread across different bacterial species?
The AI co-scientist generated five ranked hypotheses. Its top-ranked suggestion was that cf-PICIs achieve their broad host range through “capsid-tail interactions,” proposing that the cf-PICI heads could interact with a wide range of phage tails. This hypothesis almost perfectly mirrored the “tail piracy” mechanism the human team had spent years discovering.
The AI, unburdened by the researchers’ initial assumptions and biases from existing scientific models, arrived at the core of the discovery in a matter of days. When the researchers benchmarked this result, they found that other leading AI models were not able to produce the same correct hypothesis, suggesting a more advanced reasoning capability in the AI co-scientist system.
Limitations and the Path Forward
Despite these promising results, researchers involved in the work caution that significant limitations remain. The performance of the AI co-scientist has so far been evaluated on a small number of specific biological problems. More testing is needed to determine if this capability can be generalized across other scientific domains. The AI’s reasoning is also dependent on the quality and completeness of the publicly available data it analyzes, which may contain its own biases or gaps in knowledge.
Perhaps most importantly, human expertise remains essential. While an AI can generate a large volume of plausible hypotheses, it lacks the deep contextual judgment that comes from years of hands-on experience. An experienced scientist is still needed to evaluate which ideas are truly worth pursuing and to design the precise experiments required for validation. The challenge of how to prioritize AI-generated ideas is substantial, as traditional experimental pipelines are not fast or inexpensive enough to test every promising lead.
“Generally, AI output must be evaluated by people with knowledge in the area; and AI output is most valuable to those with domain-specific expertise because they are best positioned to assess it and to make use of it,” Peltz told PsyPost.
Nevertheless, these two studies provide evidence that AI systems are evolving from helpful assistants into true collaborative partners in the scientific process. By generating novel and experimentally verifiable hypotheses, tools like the AI co-scientist have the potential to supercharge human intuition and accelerate the pace of scientific and biomedical breakthroughs.
“I believe that AI will dramatically accelerate the pace of discovery for many biomedical areas and will soon be used to improve patient care,” Peltz said. “My lab is currently using it for genetic discovery and for drug re-purposing, but there are many other areas of bioscience that will soon be impacted. At present, I believe that AI co-scientist is the best in this area, but this is a rapidly advancing field.”
The study, “AI-Assisted Drug Re-Purposing for Human Liver Fibrosis,” was authored by Yuan Guan, Lu Cui, Jakkapong Inchai, Zhuoqing Fang, Jacky Law, Alberto Alonzo Garcia Brito, Annalisa Pawlosky, Juraj Gottweis, Alexander Daryin, Artiom Myaskovsky, Lakshmi Ramakrishnan, Anil Palepu, Kavita Kulkarni, Wei-Hung Weng, Zhuanfen Cheng, Vivek Natarajan, Alan Karthikesalingam, Keran Rong, Yunhan Xu, Tao Tu, and Gary Peltz.
The study, “Chimeric infective particles expand species boundaries in phage-inducible chromosomal island mobilization,” was authored by Lingchen He, Jonasz B. Patkowski, Jinlong Wang, Laura Miguel-Romero, Christopher H.S. Aylett, Alfred Fillol-Salom, Tiago R.D. Costa, and José R. Penadés.
The study, “AI mirrors experimental science to uncover a mechanism of gene transfer crucial to bacterial evolution,” was authored by José R. Penadés, Juraj Gottweis, Lingchen He, Jonasz B. Patkowski, Alexander Daryin, Wei-Hung Weng, Tao Tu, Anil Palepu, Artiom Myaskovsky, Annalisa Pawlosky, Vivek Natarajan, Alan Karthikesalingam, and Tiago R.D. Costa.