New $2 saliva test may aid in psychiatric diagnosis
A team of researchers in Brazil has engineered an inexpensive, disposable sensor that can detect a key protein linked to mental health conditions using a drop of saliva. Published in the journal ACS Polymers Au, the device could one day offer a rapid, non-invasive tool to help in the diagnosis and monitoring of disorders like depression and schizophrenia. The results are available in under an hour, offering a significant departure from current lab-based methods.
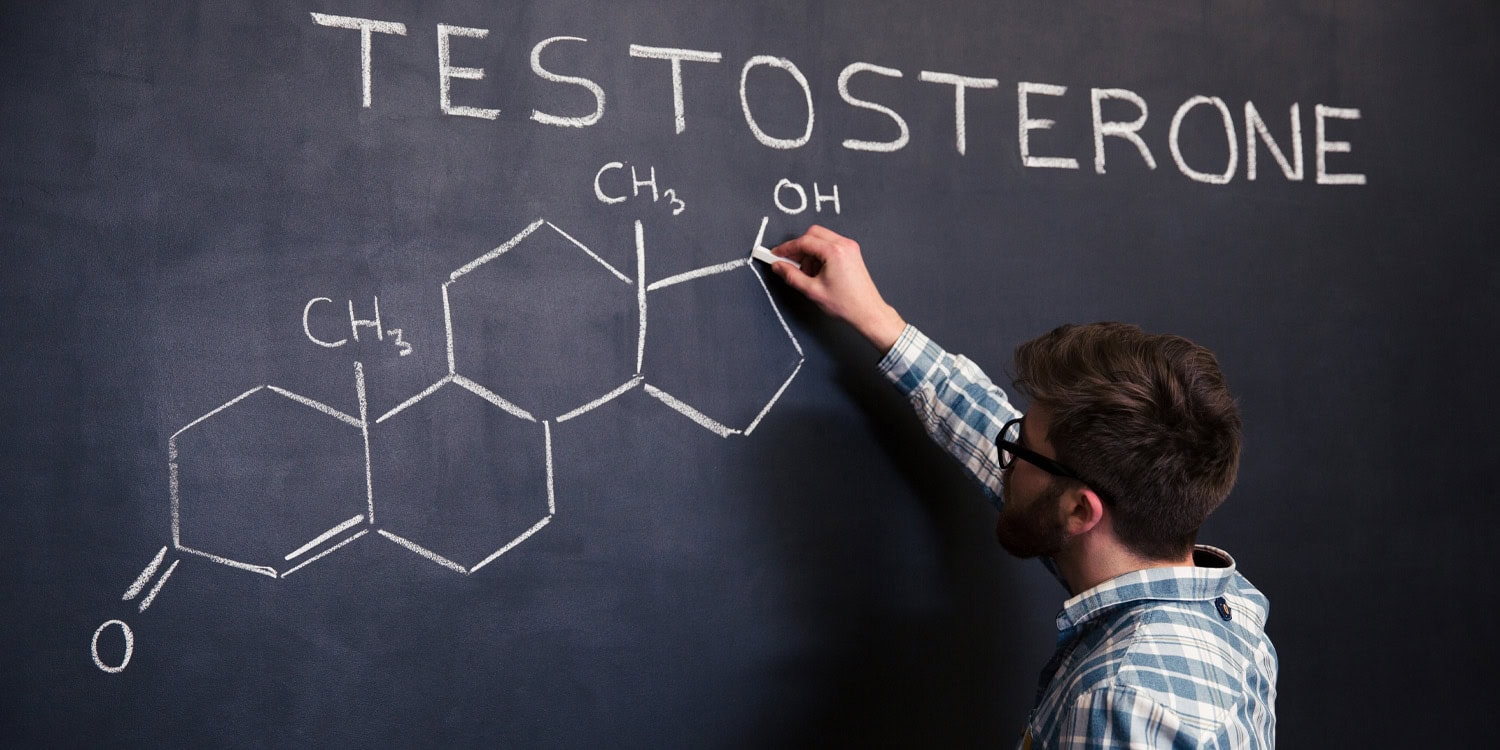
Diagnosing and managing psychiatric disorders currently relies heavily on clinical interviews and patient-reported symptoms, which can be subjective. Scientists have been searching for objective biological markers, and a protein called brain-derived neurotrophic factor, or BDNF, has emerged as a promising candidate. Lower-than-normal levels of BDNF, which supports the health and growth of neurons, have been consistently associated with conditions like major depression, bipolar disorder, and schizophrenia.
Existing methods for measuring BDNF typically involve blood draws and rely on complex, time-consuming laboratory procedures like the enzyme-linked immunosorbent assay. These techniques are often expensive and require specialized equipment and personnel, making them impractical for routine clinical use or for monitoring patient progress outside of a dedicated lab. The researchers sought to develop a fast, affordable, and non-invasive alternative that could be used at the point of care, motivated by the global increase in mental health conditions.
The foundation of the device is a small, flexible strip of polyester, similar to a piece of plastic film. Using a screen-printing technique, the scientists printed three electrodes onto this strip using carbon- and silver-based inks. This fabrication method is common in electronics and allows for inexpensive, mass production of the sensor strips.
To make the sensor specific to BDNF, the team modified the surface of the main working electrode in a multi-step process. First, they coated it with a layer of microscopic carbon spheres, which are synthesized from a simple glucose solution. This creates a large, textured surface area that is ideal for anchoring other molecules and enhances the sensor’s electrical sensitivity.
Next, they added a sequence of chemical layers that act as a sticky foundation for the biological components. Onto this foundation, they attached specialized proteins called antibodies. These anti-BDNF antibodies are engineered to recognize and bind exclusively to the BDNF protein, much like a key fits into a specific lock. A final chemical layer was added to block any remaining empty spots on the surface, which prevents other molecules in saliva from interfering with the measurement.
When a drop of saliva is applied to the sensor, any BDNF protein present is captured by the antibodies on the electrode. This binding event physically alters the electrode’s surface, creating a minute barrier that impedes the flow of electrons. The device then measures this change by sending a small electrical signal through the electrode and recording its resistance to that signal.
A greater amount of captured BDNF creates a larger barrier, resulting in a higher resistance, which can be precisely quantified. The entire process, from sample application to result, can be completed in about 35 minutes. The data is captured by a portable analyzer that can communicate wirelessly with a device like a smartphone, allowing for real-time analysis.
The research team demonstrated that their biosensor was remarkably sensitive. It could reliably detect BDNF across a vast concentration range, from incredibly minute amounts (as low as 10⁻²⁰ grams per milliliter) up to levels typically seen in healthy individuals.
This wide detection range is significant because it means the device could potentially identify the very low BDNF levels that may signal a disorder. It could also track the increase in BDNF levels as a patient responds positively to treatment, such as antidepressants, offering an objective measure of therapeutic success.
The sensor also proved to be highly selective. When tested against a variety of other substances commonly found in saliva, including glucose, uric acid, paracetamol, and even the spike protein from the SARS-CoV-2 virus, the device did not produce a false signal. It responded specifically to BDNF, confirming the effectiveness of its design.
Furthermore, tests using human saliva samples that were supplemented with known quantities of the protein showed that the sensor could accurately measure BDNF levels even within this complex biological fluid. The researchers estimated the cost of the materials for a single disposable strip to be around $2.19, positioning it as a potentially accessible diagnostic tool.
The current study was a proof-of-concept and has certain limitations. The experiments were conducted with a limited number of saliva samples from a single volunteer, which were then modified in the lab to contain varying concentrations of the target protein.
The next essential step will be to test the biosensor with a large and diverse group of patients diagnosed with various psychiatric conditions to validate its accuracy and reliability in a real-world clinical setting. Such studies would be needed to establish clear thresholds for what constitutes healthy versus potentially pathological BDNF levels in saliva. The researchers also plan to secure a patent for their technology and refine the device for potential commercial production. Future work could also explore integrating sensors for other biomarkers onto the same strip, allowing for a more comprehensive health assessment from a single saliva sample.
The study, “Low-Cost, Disposable Biosensor for Detection of the Brain-Derived Neurotrophic Factor Biomarker in Noninvasively Collected Saliva toward Diagnosis of Mental Disorders,” was authored by Nathalia O. Gomes, Marcelo L. Calegaro, Luiz Henrique C. Mattoso, Sergio A. S. Machado, Osvaldo N. Oliveira Jr., and Paulo A. Raymundo-Pereira.